Бабезиоз
| Бабезиоз | |
|---|---|
| Другие имена | Бабезиаз, Техасская лихорадка |
 | |
| Мазок крови из Babesia microti | |
| Произношение |
|
| Специальность | Инфекционная болезнь |
| Симптомы | Лихорадка , озноб , головная боль, усталость [ 1 ] |
| Risk factors | Removed spleen, weakened immune system, doing outdoor activities[1] |
| Differential diagnosis | Malaria |
Бабезиоз или пироплазмоз представляет собой малярию, подобное паразитовому заболеванию, вызванное инфекцией эукариотическим паразитом в порядке пиропласмиды , как правило, кабезия или тилерия , в Phylum apicomplexa . [ 2 ] Передача кабезиоза человека с помощью укуса клеща наиболее распространена в северо -восточном и Среднем Западе Соединенных Штатов и в некоторых частях Европы, а также спорадическая во всем остальном мире. Это происходит в теплую погоду. [ 3 ] Люди могут заразиться паразитами Бабезии укусом зараженного клеща , получая переливание крови от зараженного донора продуктов крови или врожденной передачей (зараженная мать ее ребенка). [ 4 ] Клещи передают человеческий штамм бабезиоза, поэтому он часто приводит к другим заболеваниям клещей, таким как болезнь Лайма . [ 5 ] После трипаносомов . Бабезия считается вторым по самым распространенным паразитам крови млекопитающих Они могут оказывать серьезное неблагоприятное воздействие на здоровье домашних животных в районах без сильной зимы. У крупного рогатого скота болезнь известна как техасская лихорадка крупного рогатого скота или красная вода . [ 6 ]
Signs and symptoms
[edit]Half of all children and a quarter of previously healthy adults with Babesia infection are asymptomatic. When people do develop symptoms, the most common are fever and hemolytic anemia, symptoms that are similar to those of malaria.[5] People with symptoms usually become ill 1 to 4 weeks after the bite, or 1 to 9 weeks after transfusion of contaminated blood products. A person infected with babesiosis gradually develops malaise and fatigue, followed by a fever. Hemolytic anemia, in which red blood cells are destroyed and removed from the blood, also develops. Chills, sweats, and thrombocytopenia are also common symptoms. Symptoms may last from several days to several months.[7]
Less common symptoms and physical exam findings of mild-to-moderate babesiosis:[5]
- Headache
- Muscle pain
- Anorexia
- Nonproductive cough (mucus is not coughed up)
- Arthralgias (noninflammatory joint pain, unlike arthritis, which is inflammatory)
- Nausea
- Vomiting
- Sore throat
- Abdominal pain
- Pink eye/Conjunctivitis
- Photophobia (abnormal intolerance to visual perception of light)
- Weight loss
- Emotional lability
- Depression
- Hyperesthesia (more sensitive to stimuli)
- Enlarged spleen
- Pharyngeal erythema
- Enlarged liver
- Jaundice (yellowing of the skin and of the sclera)
- Retinopathy with splinter hemorrhages
- Retinal infarcts
- Neutropenia[8]
In more severe cases, symptoms similar to malaria occur, with fevers up to 40.5 °C (105 °F), shaking chills, and severe anemia (hemolytic anemia). Organ failure may follow, including adult respiratory distress syndrome. Sepsis in people who have had a splenectomy can occur rapidly, consistent with overwhelming post-splenectomy infection. Severe cases are also more likely to occur in the very young, very old, and persons with immunodeficiency, such as HIV/AIDS patients.[9]
A reported increase in human babesiosis diagnoses in the 2000s is thought to be caused by more widespread testing and higher numbers of people with immunodeficiencies coming in contact with ticks, the disease vector.[6] Little is known about the occurrence of Babesia species in malaria-endemic areas, where Babesia can easily be misdiagnosed as Plasmodium. Human patients with repeat babesiosis infection may exhibit premunity.[10]
Cause
[edit]Babesia species are in the phylum Apicomplexa, which also has the protozoan parasites that cause malaria, toxoplasmosis, and cryptosporidiosis.[5] Four clades of Babesia species infect humans. The main species in each clade are:[citation needed]
- B. microti (< 3 μm)
- B. duncani
- B. divergens (cattle parasite seen mostly in Europe) and B. venatorum (roe deer parasite, formerly called EU1), most closely related to the large Babesia clade
- Large Babesia (> 3 μm) mostly infects ungulates, but also includes K01 strain (an isolated case observed in South Korea, see isolated cases)
Pathophysiology
[edit]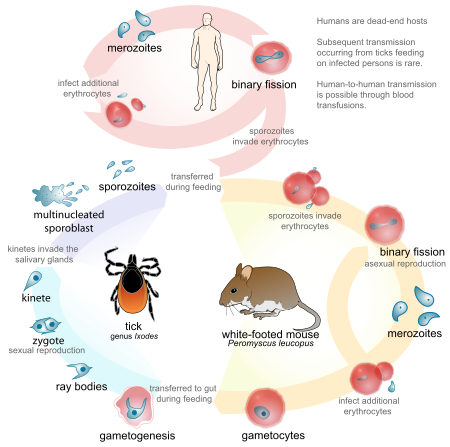
Babesia parasites reproduce in red blood cells, where they can be seen as cross-shaped inclusions (four merozoites asexually budding, but attached together forming a structure looking like a "Maltese cross")[11] and cause hemolytic anemia, quite similar to malaria.
Unlike the Plasmodium parasites that cause malaria, Babesia species almost never exhibit an exoerythrocytic phase with trophozoite forms.[12]
In nonhuman animals, Babesia canis rossi, Babesia bigemina, and Babesia bovis cause particularly severe forms of the disease, including a severe haemolytic anaemia, with positive erythrocyte-in-saline-agglutination test indicating an immune-mediated component to the haemolysis. Common sequelae include haemoglobinuria "red-water", disseminated intravascular coagulation, and "cerebral babesiosis" caused by sludging of erythrocytes in cerebral capillaries.[citation needed]
In bovine species, the organism causes hemolytic anemia, so an infected animal shows pale mucous membranes initially. As the levels of bilirubin (a byproduct of red blood cell lysis) continue to increase, the visible mucous membranes become yellow in color (icterus) due to the failure of the liver to metabolize the excess bilirubin. Hemoglobinuria is seen due to excretion of red-blood-cell lysis byproducts via the kidneys. Fever of 40.5 °C (105 °F) develops due to release of inflammatory byproducts.[citation needed]
Diagnosis
[edit]Only specialized laboratories can adequately diagnose Babesia infection in humans, so Babesia infections are considered highly under-reported. It develops in patients who live in or travel to an endemic area or receive a contaminated blood transfusion within the preceding 9 weeks, so this aspect of the medical history is vital.[13] Babesiosis may be suspected when a person with such an exposure history develops persistent fevers and hemolytic anemia. The definitive diagnostic test is the identification of parasites on a Giemsa-stained thin-film blood smear.[13]
So-called "Maltese cross formations" on the blood film are diagnostic (pathognomonic) of babesiosis, since they are not seen in malaria, the primary differential diagnosis.[11] Careful examination of multiple smears may be necessary, since Babesia may infect less than 1% of circulating red blood cells, thus be easily overlooked.[14]
Serologic testing for antibodies against Babesia (both IgG and IgM) can detect low-level infection in cases with a high clinical suspicion, but negative blood film examinations. Serology is also useful for differentiating babesiosis from malaria in cases where people are at risk for both infections. Since detectable antibody responses require about a week after infection to develop, serologic testing may be falsely negative early in the disease course.[15]
A polymerase chain reaction (PCR) test has been developed for the detection of Babesia from the peripheral blood.[16] PCR may be at least as sensitive and specific as blood-film examination in diagnosing babesiosis, though it is also significantly more expensive.[17] Most often, PCR testing is used in conjunction with blood film examination and possibly serologic testing.[13]
Other laboratory findings include decreased numbers of red blood cells and platelets on complete blood count.[18]
In animals, babesiosis is suspected by observation of clinical signs (hemoglobinuria and anemia) in animals in endemic areas. Diagnosis is confirmed by observation of merozoites on thin film blood smear examined at maximum magnification under oil using Romonovski stains (methylene blue and eosin). This is a routine part of the veterinary examination of dogs and ruminants in regions where babesiosis is endemic.[citation needed]
Babesia canis and B. bigemina are "large Babesia species" that form paired merozoites in the erythrocytes, commonly described as resembling "two pears hanging together", rather than the "Maltese cross" of the "small Babesia species". Their merozoites are around twice the size of small ones.[citation needed]
Cerebral babesiosis is suspected in vivo when neurological signs (often severe) are seen in cattle that are positive for B. bovis on blood smear, but this has yet to be proven scientifically. Outspoken red discoloration of the grey matter post mortem further strengthens suspicion of cerebral babesiosis. Diagnosis is confirmed post mortem by observation of Babesia-infected erythrocytes sludged in the cerebral cortical capillaries in a brain smear.[citation needed]
Treatment
[edit]Treatment of asymptomatic carriers should be considered if parasites are still detected after 3 months. In mild-to-moderate babesiosis, the treatment of choice is a combination of atovaquone and azithromycin. This regimen is preferred to clindamycin and quinine because it has fewer side effects. The standard course is 7 to 10 days, but this is extended to at least 6 weeks in people with relapsing disease. Even mild cases are recommended to be treated to decrease the chance of inadvertently transmitting the infection by donating blood.[5] In severe babesiosis, the combination of clindamycin and quinine is preferred. In life-threatening cases, exchange transfusion is performed.[19] In this procedure, the infected red blood cells are removed and replaced with uninfected ones; toxins produced by the parasites may also be removed.[20]
Imidocarb is a drug used for treatment of babesiosis in dogs.[21] Extracts of the poisonous, bulbous plant Boophone disticha are used in the folk medicine of South Africa to treat equine babesiosis. B. disticha is a member of the daffodil family Amaryllidaceae and has also been used in preparations employed as arrow poisons, hallucinogens, and in embalming. The plant is rich in alkaloids, some of which display an action similar to that of scopolamine.[22]
Epidemiology
[edit]Babesiosis is a vector-borne illness usually transmitted by Ixodes scapularis ticks. B. microti uses the same tick vector as Lyme disease, and may occur in conjunction with Lyme.[6] The organism can also be transmitted by blood transfusion.[23][24] Ticks of domestic animals, especially Rhipicephalus (Boophilus) microplus and R. (B.) decoloratus transmit several species of Babesia to livestock, causing considerable economic losses to farmers in tropical and subtropical regions.[citation needed]
In the United States, the majority of babesiosis cases are caused by B. microti, and occur in the Northeast and northern Midwest from May through October.[5] Areas with especially high rates include eastern Long Island, Fire Island, Nantucket Island, and Martha's Vineyard.[25][26][27][28][29] The Centers for Disease Control and Prevention now requires state health departments to report infections using Form OMB No. 0920-0728.[30] In 2014, Rhode Island had an incidence of 16.3 reported infections per 100,000 people.[31]
In Europe, B. divergens is the primary cause of infectious babesiosis and is transmitted by I. ricinus.[5]
Babesiosis has emerged in Lower Hudson Valley, New York, since 2001.[32]
In Australia, one locally-acquired case of B. microti has been reported, which was fatal.[33] A subsequent investigation found no additional evidence of human Babesiosis in over 7000 patient samples, leading the authors to conclude that Babesiosis was rare in Australia.[34] A similar disease in cattle, commonly known as tick fever, is spread by Babesia bovis and B. bigemina in the introduced cattle tick Rhipicephalus microplus. This disease is found in eastern and northern Australia.[35]
Isolated cases
[edit]A table of isolated cases of babesiosis, which may be underestimated given how widely distributed the tick vectors are in temperate latitudes.[5]
| Location | Species |
|---|---|
| Pacific Coast (northern California to Washington) | B. duncani |
| Kentucky, Missouri, and Washington | B. divergens |
| Austria, Germany, Italy | B. venatorum |
| Canary Islands | B. microti |
| Africa (Egypt, Mozambique, South Africa) | Uncharacterized spp. |
| Asia (Taiwan, Japan) | B. microti |
| South Korea | Babesia KO1[36] |
| Australia | B. microti[34] |
| South America (Brazil, Colombia) | Uncharacterized spp. |
History
[edit]The disease is named for the genus of the causative organism,[37] which was named after the Romanian bacteriologist Victor Babeș.[38] In 1888, Victor Babeș identified the microorganisms in red blood cells as the cause of febrile hemoglobinuria in cattle.[5] In 1893, Theobald Smith and Frederick Kilborne discovered that a tick was the vector for transmission in Texas cattle. The agent was B. bigemina. This was the first demonstration that an arthropod could act as a disease vector to transmit an infectious agent to a vertebrate host.[citation needed]
In 1957, the first human case was documented in a splenectomized Croatian herdsman.[5] The agent was B. divergens. In 1969, the first case was reported in an immunocompetent individual on Nantucket Island. The agent was B. microti, and the vector was the tick I. scapularis.[citation needed] Equine babesiosis (caused by the protozoan Theileria equi) is also known as piroplasmosis (from the Latin piro, meaning pear + Greek plasma, a thing formed).[39]
Other animals
[edit]Veterinary treatment of babesiosis does not normally use antibiotics. In livestock and animals, diminazen (Berenil), imidocarb, or trypan blue would be the drugs of choice for treatment of B. canis rossi (dogs in Africa), B. bovis, and B. bigemina (cattle in Southern Africa). In acute cases in cattle, blood transfusion may be carried out. A vaccine is effective against B. canis canis (dogs in the Mediterranean region), but is ineffective against B. c. rossi. B. imitans causes a mild form of the disease that frequently resolves without treatment (dogs in Southeast Asia).[citation needed]
References
[edit]- ^ Jump up to: a b "CDC - Babesiosis". Centers for Disease Control and Prevention. Archived from the original on 2021-03-08. Retrieved 2021-02-25.
- ^ Berger SA, Marr JS (2006). Human Parasitic Diseases Sourcebook. Jones & Bartlett Learning. ISBN 978-0-7637-2962-2. Archived from the original on 2013-11-13. Retrieved 2016-10-14.
- ^ Prevention CC. "CDC - Babesiosis". www.cdc.gov. Archived from the original on 2015-10-25. Retrieved 2015-10-25.
- ^ Prevention CC. "CDC2 - Babesiosis" (PDF). www.cdc.gov. Archived (PDF) from the original on 2018-07-27. Retrieved 2018-09-20.
- ^ Jump up to: a b c d e f g h i j Vannier E, Krause PJ (21 June 2012). "Human Babesiosis" (PDF). New England Journal of Medicine. 366 (25): 2397–2407. doi:10.1056/NEJMra1202018. PMID 22716978. S2CID 205116383. Archived (PDF) from the original on 2021-11-12.
- ^ Jump up to: a b c Hunfeld KP, Hildebrandt A, Gray JS (2008). "Babesiosis: Recent insights into an ancient disease". Int J Parasitol. 38 (11): 1219–37. doi:10.1016/j.ijpara.2008.03.001. PMID 18440005.
- ^ Marcos LA, Wormser GP. Relapsing Babesiosis With Molecular Evidence of Resistance to Certain Antimicrobials Commonly Used to Treat Babesia microti Infections. Open Forum Infect Dis. 2023 Jul 20;10(8):ofad391. doi: 10.1093/ofid/ofad391. PMID: 37539067; PMCID: PMC10394720.
- ^ Wormser GP, et al. (2015). "Neutropenia in congenital and adult babesiosis". Am J Clin Pathol. 144 (1): 94–96. doi:10.1309/AJCP2PHH4HBVHZFS. PMID 26071466. Archived from the original on 2019-12-18. Retrieved 2015-08-19.
- ^ Lobo CA, Singh M, Rodriguez M. Human babesiosis: recent advances and future challenges. Curr Opin Hematol. 2020 Nov;27(6):399-405. doi: 10.1097/MOH.0000000000000606. PMID: 32889826; PMCID: PMC11042670.
- ^ Shaw SE, Day MJ (11 April 2005). Arthropod-borne Infectious Diseases of the Dog and Cat. Manson Publishing. p. 71. ISBN 978-1-84076-578-6. Archived from the original on 26 June 2014. Retrieved 14 October 2016.
- ^ Jump up to: a b Noskoviak K, Broome E (2008). "Images in clinical medicine. Babesiosis". N Engl J Med. 358 (17): e19. doi:10.1056/NEJMicm070903. PMID 18434647.
- ^ Setty S, Khalil Z, Schori P, Azar M, Ferrieri P. Babesiosis. Two atypical cases from Minnesota and a review. Am J Clin Pathol. 2003 Oct;120(4):554-9. doi: 10.1309/N3DP-9MFP-NUJD-4XJY. PMID: 14560566.
- ^ Jump up to: a b c Wormser GP, Dattwyler RJ, Shapiro ED, et al. (November 2006). "The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America" (PDF). Clin. Infect. Dis. 43 (9): 1089–134. doi:10.1086/508667. PMID 17029130. Archived (PDF) from the original on 2020-07-26. Retrieved 2019-09-20.
- ^ Krause PJ (2003). "Babesiosis diagnosis and treatment". Vector Borne Zoonotic Dis. 3 (1): 45–51. doi:10.1089/153036603765627451. PMID 12804380.
- ^ Krause PJ, Telford SR, Ryan R, et al. (April 1994). "Diagnosis of babesiosis: evaluation of a serologic test for the detection of Babesia microti antibody". J. Infect. Dis. 169 (4): 923–6. doi:10.1093/infdis/169.4.923. PMID 8133112.
- ^ Persing DH, Mathiesen D, Marshall WF, et al. (August 1992). "Detection of Babesia microti by polymerase chain reaction". J. Clin. Microbiol. 30 (8): 2097–103. doi:10.1128/jcm.30.8.2097-2103.1992. PMC 265450. PMID 1500517.
- ^ Krause PJ, Telford S, Spielman A, et al. (November 1996). "Comparison of PCR with blood smear and inoculation of small animals for diagnosis of Babesia microti parasitemia". J. Clin. Microbiol. 34 (11): 2791–4. doi:10.1128/jcm.34.11.2791-2794.1996. PMC 229405. PMID 8897184.
- ^ Akel T, Mobarakai N. Hematologic manifestations of babesiosis. Ann Clin Microbiol Antimicrob. 2017 Feb 15;16(1):6. doi: 10.1186/s12941-017-0179-z. PMID: 28202022; PMCID: PMC5310009.
- ^ Таниэль Е., Гюлер Н., Хокелек М., Ульджер Ф., Санбул М. (2015). «Случай тяжелого бабезиоза, успешно лечившись с помощью переливания обмена» . Int J Infect dis . 38 : 83–5. doi : 10.1016/j.ijid.2015.07.019 . PMID 26232090 .
- ^ Saifee NH, Krause PJ, Wu Y. Аферез для бабезиоза: терапевтическое восстановление паразита или удаление вредных токсинов или обоих? J Clin Apher. 2016 октября; 31 (5): 454-8. doi: 10.1002/jca.21429. Epub 2015 20 октября. PMID: 26481763.
- ^ «Имизол | Обзор» . Здоровье животных Merck. Архивировано из оригинала 7 августа 2015 года . Получено 15 августа 2015 года .
- ^ Герцог JA . « Буфон дивистах» (Liliaceae) » . Фитохимические и этноботанические базы данных доктора Дьюка. Архивировано с оригинала 15 января 2018 года . Получено 10 ноября 2011 года .
- ^ Herwaldt BL, Linden JV, Bosserman E, Young C, Olkowska D, Wilson M (2011). «Бабезиоз, связанный с трансфузией в Соединенных Штатах: описание случаев». Ann Interned Med . 155 (8): 509–19. doi : 10.7326/0003-4819-155-8-201110180-00362 . PMID 21893613 . S2CID 74852997 .
- ^ Лейби Д.А. (2011). «Бабезиоз, связанный с трансфузией: разве мы не должны быть отмечены?». Ann Interned Med . 155 (8): 556–7. doi : 10.7326/0003-4819-155-8-201110180-00363 . PMID 21893616 . S2CID 807441 .
- ^ Джаннини А.Дж., Блэк Хр, Геттсше Р.Л. (1978). Справочник по психиатрическим, психогенным и соматопсихическим расстройствам: лабораторное и клиническое руководство по медицинскому лечению эмоциональной и интеллектуальной патологии . Медицинское обследование. п. 86. ISBN 978-0-87488-596-5 Полем Архивировано из оригинала 2020-07-26 . Получено 2016-10-14 .
- ^ Belluck P (6 сентября 2009 г.). «У болезни с клещами есть нантакет, учитывая некоторые решения на основе оленей» . New York Times . Архивировано с оригинала 15 ноября 2011 года . Получено 6 сентября 2009 г.
- ^ Herwaldt BL, Persing DH, Precigout EA, et al. (1996). «Фатальный случай бабезиоза в Миссури: выявление другой пироплазмы, которая заражает людей». Анналы внутренней медицины . 124 (7): 643–50. doi : 10.7326/0003-4819-124-7-199604010-00004 . PMID 8607592 . S2CID 46733758 .
- ^ Mylonakis E (май 2001 г.). «Когда подозревать и как следить за бабезиозом» . Am Fam Врач . 63 (10): 1969–74. PMID 11388711 . Архивировано из оригинала 2022-07-21 . Получено 2012-05-26 .
- ^ "Babesiosis Faqs" . Центры по контролю и профилактике заболеваний (CDC. 5 мая 2009 года. Архивировано с оригинала 28 ноября 2010 года . Получено 6 сентября 2009 г.
- ^ «Паразиты - Бабезиоз: национальное наблюдение» . Центры для контроля и профилактики заболеваний . Архивировано из оригинала 16 декабря 2017 года . Получено 19 июня 2018 года .
- ^ Центры для контроля и профилактики заболеваний. «Данные и статистика» . Центр Архивировано с оригинала 19 июня 2018 года . Получено 19 июня 2018 года .
- ^ Джозеф Дж. Т., Рой С.С., Шамс Н., Вистинтинер П., Надельман Р.Б., Хосур С. и др. (Май 2011). «Бабезиоз в Нижней долине Гудзона, Нью -Йорк, США» . Emerge Infect Dis . 17 (5): 843–7. doi : 10.3201/eid1705.101334 . PMC 3321771 . PMID 21529393 .
Связанные новостные статьи: Лори Таркан (20 июня 2011 г.). «Однажды редко, инфекция от укусов клещей распространяется» . New York Times . Архивировано с оригинала 25 ноября 2016 года . Получено 24 февраля 2017 года . - ^ Senanayake SN, Paparini A, Latimer M, Andriolo K, Dasilva AJ, Wilson H, et al. (March 2012). "First report of human babesiosis in Australia". Medical Journal of Australia. 196 (5): 350–352. doi:10.5694/mja11.11378. PMID 22432676. S2CID 33068508.
- ^ Jump up to: а беременный Faddy HM, Rooks KM, Irwin PJ, Viennet E, Paparini A, Seed CR, et al. (Июль 2019). «Нет никаких доказательств широко распространенной передачи микроти в Австралии». Переливание . 59 (7): 2368–2374. doi : 10.1111/trf.15336 . PMID 31070793 . S2CID 148570372 .
- ^ Правительство Квинсленда, Департамент первичных отраслей и рыболовства. «Лихорадка (бычий бабезиоз)» . Архивировано из оригинала 5 апреля 2011 года . Получено 21 февраля 2012 года .
- ^ Kim JY, Cho SH, Joo HN, et al. (Июнь 2007 г.). «Первый случай человеческого кабезиоза в Корее: обнаружение и характеристика нового типа Бабезии sp. (KO1), похожий на овайн -Бабезию» . J. Clin. Микробиол . 45 (6): 2084–7. doi : 10.1128/jcm.01334-06 . PMC 1933034 . PMID 17392446 .
- ^ "Бабезия" Аархивирована 2022-04-24 на машине Wayback в Merriam-Webster Online.
- ^ Виктор Бабș в том, кто его назвал?
- ^ «Определение пироплазмы» . Lexic.us. Архивировано с оригинала 11 ноября 2011 года . Получено 9 ноября 2011 года .
Внешние ссылки
[ редактировать ]- Центр глобального здравоохранения (2019-06-25). «Бабезиоз» . Паразиты и здравоохранение, DPDX - Лабораторная идентификация паразитов по вопросам общественного здравоохранения . Центры для контроля и профилактики заболеваний. Архивировано из оригинала 2013-03-07 . Получено 2003-10-07 . Источник общественного достояния , из которого была получена первая версия этой статьи.
- Krause PJ, Auwaerter PG, Bannuru RR, Branda JA, Falck-yter YT, Lantos PM, et al. (27 января 2021 г.). «Руководство по клинической практике, проведенное Обществом Америки инфекционных заболеваний (IDSA): Руководство 2020 года по диагностике и лечению Babesisis » Клинические инфекционные заболевания 72 (2): E49 - E6 Doi : 10.1093/ cid/ ciaa1 33252652PMID
- Гомер М.Дж., Агилар-Делфин I, Телфорд С.Р., Краузе П.Дж., Персинг Д.Х. (июль 2000 г.). «Бабезиоз» . Клин Микробиол. Преподобный 13 (3): 451–69. doi : 10.1128/cmr.13.3.451-469.2000 . PMC 88943 . PMID 10885987 .
- «Бабезиоз: обзор» - ветеринарное руководство Merck
- Текущий состояние конного пироплазмоза во всем мире в OIE. Интерфейс Wahid - база данных о здоровье животных в Wahid
- Карта заболевания - oie